Ataxia is a neurological sign and symptom that consists of gross lack of coordination of muscle movements. Ataxia is a non-specific clinical manifestation implying dysfunction of the parts of the nervous system that coordinate movement, such as the cerebellum. Several possible causes exist for these patterns of neurological dysfunction. The term "dystaxia" is a rarely used synonym.
The term cerebellar ataxia is used to indicate ataxia that is due to dysfunction of the cerebellum. This causes a variety of elementary neurological deficits, such as antagonist hypotonia, asynergy, dysmetria, dyschronometria, and dysdiadochokinesia. How and where these abnormalities manifest themselves depends on which cerebellar structures have been damaged, and whether the lesion is bilateral or unilateral.
- Dysfunction of the vestibulocerebellum impairs the balance and the control of eye movements. This presents itself with postural instability, in which the person tends to separate his/her feet upon standing, in order to gain a wider base and to avoid titubation (bodily oscillations tending to be forward-backward ones). The instability is therefore worsened when standing with the feet together, regardless of whether the eyes are open or closed. This is a negative Romberg's test, or more accurately, it denotes the individual's inability to carry out the test, because the individual feels unstable even with open eyes.
- Dysfunction of the spinocerebellum presents itself with a wide-based "drunken sailor" gait (called truncal ataxia), characterised by uncertain starts and stops, lateral deviations, and unequal steps.
- Dysfunction of the cerebrocerebellum presents as disturbances in carrying out voluntary, planned movements by the extremities (called appendicular ataxia). These include:
- intention tremor (coarse trembling, accentuated over the execution of voluntary movements, possibly involving the head and eyes as well as the limbs and torso);
- peculiar writing abnormalities (large, unequal letters, irregular underlining);
- a peculiar pattern of dysarthria (slurred speech, sometimes characterised by explosive variations in voice intensity despite a regular rhythm).
- inability to perform rapidly alternating movements, known as dysdiadochokinesia. This could involve rapidly switching from pronation to supination of the forearm. Movements become more irregular with increases of speed.
- inability to judge distances or ranges of movement. This is known is dysmetria and is often seen as undershooting, hypometria, or overshooting, hypermetria, the required distance or range to reach a target. This is sometimes seen when a patient is asked to reach out and touch someone's finger or touch their own nose.
- the rebound phenomenon, also known as the loss of the check reflex is also sometimes seen in patients with cerebellar ataxia. For example, when a patient is flexing their elbow isometrically against a resistance. When the resistance is suddenly removed without warning, the patient's arm may swing up and even strike themselves. With an intact check reflex, the patient will check and activate the opposing triceps to slow and stop the movement.
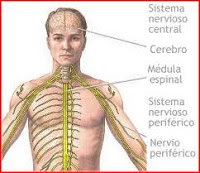
The term sensory ataxia is employed to indicate ataxia due to loss of proprioception, the loss of sensitivity to the positions of joint and body parts. This is generally caused by dysfunction of the dorsal columns of the spinal cord, because they carry proprioceptive information up to the brain. In some cases, the cause of sensory ataxia may instead be dysfunction of the various parts of the brain which receive positional information, including the cerebellum, thalamus, and parietal lobes.
Sensory ataxia presents itself with an unsteady "stomping" gait with heavy heel strikes, as well as a postural instability that is usually worsened when the lack of proprioceptive input cannot be compensated for by visual input, such as in poorly lit environments.
Physicians can find evidence of sensory ataxia during physical examination by having the patient stand with his/her feet together and eyes shut. In affected patients, this will cause the instability to worsen markedly, producing wide oscillations and possibly a fall. This is called a positive Romberg's test. Worsening of the finger-pointing test with the eyes closed is another feature of sensory ataxia. Also, when the patient is standing with arms and hands extended toward the physician, if the eyes are closed, the patient's finger will tend to "fall down" and then be restored to the horizontal extended position by sudden muscular contractions (the "ataxic hand").
The term vestibular ataxia is employed to indicate ataxia due to dysfunction of the vestibular system, which in acute and unilateral cases is associated with prominent vertigo, nausea and vomiting. In slow-onset, chronic bilateral cases of vestibular dysfunction, these characteristic manifestations may be absent, and dysequilibrium may be the sole presentation.
The three types of ataxia have overlapping causes, and therefore can either coexist or occur in isolation.
Any type of focal lesion of the central nervous system (such as stroke, brain tumour, multiple sclerosis) will cause the type of ataxia corresponding to the site of the lesion: cerebellar if in the cerebellum, sensory if in the dorsal spinal cord (and rarely in the thalamus or parietal lobe), vestibular if in the vestibular system (including the vestibular areas of the cerebral cortex).
Exogenous substances that cause ataxia mainly do so because they have a depressant effect on central nervous system function. The most common example is ethanol, which is capable of causing reversible cerebellar and vestibular ataxia. Other examples include various prescription drugs (e.g. most antiepileptic drugs have cerebellar ataxia as a possible adverse effect), Lithium level over 1.5mEq/L, cannabis ingestion and various other recreational drugs (e.g. ketamine, PCP or dextromethorphan, all of which are NMDA receptor antagonists that produce a dissociative state at high doses). Exposure to high levels of methylmercury, through consumption of fish with high mercury concentrations, is also a known cause of ataxia and other neurological disorders
Peripheral neuropathies may cause generalised or localised sensory ataxia (e.g. a limb only) depending on the extent of the neuropathic involvement. Spinal disorders of various types may cause sensory ataxia from the lesioned level below, when they involve the dorsal columns.
Non-hereditary causes of cerebellar degeneration include chronic ethanol abuse, paraneoplastic cerebellar degeneration, high altitude cerebral oedema, coeliac disease, normal pressure hydrocephalus and cerebellitis.
Ataxia may depend on hereditary disorders consisting of degeneration of the cerebellum and/or of the spine; most cases feature both to some extent, and therefore present with overlapping cerebellar and sensory ataxia, even though one is often more evident than the other. Hereditary disorders causing ataxia include autosomal dominant ones such as spinocerebellar ataxia, episodic ataxia, and dentatorubropallidoluysian atrophy, as well as autosomal recessive disorders such as Friedreich's ataxia (sensory and cerebellar, with the former predominating) and Niemann Pick disease, ataxia-telangiectasia (sensory and cerebellar, with the latter predominating), and abetalipoproteinaemia. An example of X-linked ataxic condition is the rare fragile X-associated tremor/ataxia syndrome.
The treatment of ataxia and its effectiveness depend on the underlying cause. Treatment may limit or reduce the effects of ataxia, but it is unlikely to eliminate them entirely. Recovery tends to be better in individuals with a single focal injury (such as stroke or a benign tumour), compared to those who have a neurological degenerative condition. A review of the management of degenerative ataxia was published in 2009.
The movement disorders associated with ataxia can be managed by pharmacological treatments and through physical therapy and occupational therapy to reduce disability. Some drug treatments that have been used to control ataxia include: 5-hydroxytryptophan (5-HTP), idebenone, amantadine, physostigmine, L-carnitine or derivatives, trimethoprim–sulfamethoxazole, vigabatrin,phosphatidylcholine, acetazolamide, 4-aminopyridine, buspirone, and a combined coenzyme Q10 and vitamin E antioxidant therapy. Physical therapy requires a focus on adapting activity and facilitating motor learning for retraining specific functional motor patterns. Gait, coordination, and balance training are large components of therapy. Training will likely need to be intense and focused, as indicated by one study performed with stroke patients experiencing limb ataxia who underwent intensive upper limb training. Their therapy consisted of constraint-induced movement therapy which resulted in improvements of their arm function. Treatment will likely include strategies to manage difficulties with everyday activities such as walking. Gait aids (such as a cane or walker) can be provided to decrease the risk of falls associated with a balance impairment or poor coordination. Severe ataxia may eventually call for the use of a wheelchair.
In order to obtain better results, possible coexisting motor deficits need to be addressed in addition to those induced by ataxia; for example muscle weakness and decreased endurance which would lead to increasing fatigue and poorer movement patterns.
The term "ataxia" is sometimes used in a broader sense to indicate lack of coordination in some physiological process. Examples include optic ataxia (lack of coordination between visual inputs and hand movements, resulting in inability to reach and grab objects. Optic ataxia may be caused by lesions to the posterior parietal cortex. The posterior parietal cortex is responsible for combining and expressing positional information and relating it to movement. Outputs of the posterior parietal cortex include the spinal cord, brain stem motor pathways, pre-motor and pre-frontal cortex, basal ganglia and the cerebellum. Some neurons in the posterior parietal cortex are modulated by intention. Optic ataxia is usually part of Balint's syndrome, but can be seen in isolation with injuries to the superior parietal lobule, as it represents a disconnection between visual-association cortex and the frontal premotor and motor cortex), and ataxic respiration (lack of coordination in respiratory movements, usually due to dysfunction of the respiratory centres in the medulla oblongata).